The surgical procedure of Bi-Jaw Surgery typically involves the following steps:
Anesthesia: The procedure is performed under general anesthesia with nasal endotracheal intubation. Local anesthesia with lidocaine and epinephrine may also be used to minimize blood loss.
Intraoral Incision: Incisions are made inside the mouth to avoid visible facial scars. One jaw is repositioned at a time during the surgery.
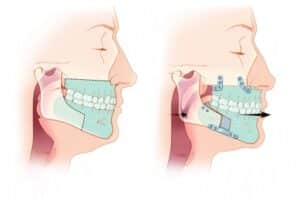
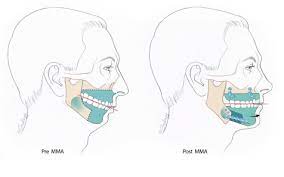
Jaw Repositioning: Depending on the patient’s needs, one or both jaws are repositioned, either brought forward or backward. Bone grafts may be used to enlarge the jaw or parts of the bone may be removed for reduction.
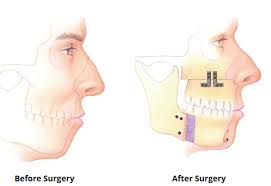
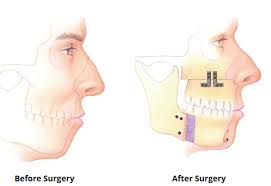
Fixation: Titanium screws and plates are used to securely hold the repositioned jaws in place. Elastic bands and wires may also be used for stabilization.
Sequence: The surgeon decides whether to work on the upper jaw (maxilla) or lower jaw (mandible) first. The sequence can vary among surgeons, but it’s commonly preferred to perform BSSO first and then LeFort osteotomy for upper jaw correction.
Bilateral Sagittal Split Osteotomy (BSSO): For BSSO, the surgeon makes cuts behind the last molar teeth diagonally and lengthwise down the jawbone, allowing the front of the jaw to move as one unit.
LeFort Osteotomy: For LeFort Osteotomy, the upper jaw is cut above the level of the tooth roots, separated from the skull and facial bones, and carefully positioned. Care is taken to avoid damage to teeth during the separation.
Fixation of Maxilla: The surgically moved maxilla is fixed to the native facial bones using plates and screws.
Closure: Incisions inside the mouth are closed in layers using absorbable sutures.
Stabilization: The jaws are not wired shut for extended periods; instead, bone segments are fixed rigidly.